
Practical Nursing alums share their stories
 by Meagan Kashty – Sep 22, 2020
by Meagan Kashty – Sep 22, 2020 Read interviews with four courageous Practical Nursing grads as they share, in their own words, what they've experienced during the COVID-19 pandemic and how their roles have changed over the past six months.
JP Munro (Practical Nursing '18)

JP Munro currently works as an RPN in the General Medicine Unit of St. Joseph’s Healthcare Hamilton.
Along with your role with St. Joseph’s in Hamilton, you also work with the Registered Practical Nurses Association of Ontario. What does that work entail?
During my last semester at Sheridan, I had a placement at the RPNAO, and it went really well, so I was offered a casual part-time position there. I’ve been working there for the past couple of years on different education initiatives, online modules, and assisting to coordinate some of their conferences. It’s a lot of different roles, but I’m always learning so it’s been a great experience so far.
We were watching the whole COVID-19 situation unfold, and a lot of people look to organizations like ours to find out their information and seek guidance. It was interesting at the beginning to be a part of that and see what’s to come.
Can you talk a bit about your work during the early days of the pandemic?
At first, there was just a lot of uncertainty. In the beginning, at least, we just kind didn't know what COVID-19 was like or what we were really dealing with. The list of symptoms was always changing and there were a lot of questions about transmission. For the most part, everyone was just kind of erring on the side of caution, which was good.
There was also a lot of concern about PPE, which I think in the end was handled quite well and prompted an amazing response. It was neat to see everyone working together, whether it be folks stitching cloth masks and donating them, or others using 3D printing to print off face shields.
One of the biggest challenges for us at the time was that patients weren't allowed to have visitors at the hospital. Oftentimes families would bring items for their family members like books, a tablet…snacks…whatever they would normally bring. So they would drop those items off at the door and then we would have to deliver them.
And then there are some patients that are in the hospital for long periods of time, so they hadn’t seen their families in months. That was one of the most difficult things for the patients, but it was also emotionally challenging for us because we could see how hard it was on our patients.
We have five patients on day shifts, and six on night shifts, and basically, we always have to balance our ability to sit and listen and chat with our patients along with a long list of tasks that need to ensure everyone’s safety. You’re really pulled in multiple directions.
How have things changed from earlier this year to now?
It’s gotten a lot easier now that restrictions have been eased, and patients can have a limited number of visitors. It’s easy to see how having family members being able to visit is really reflected in how our patients are feel.
Not even necessarily only in my role in nursing, but I feel like everyone’s come together for the most part. Everyone’s going through difficult times in their own way, and we’ve banded together. People are social distancing and wearing masks – it just shows that we care for each other, even when it’s not easy. It’s really encouraging.
Is there anything you want people to know about your experience during this time?
I know it’s not easy to social distance all the time and wear masks, but we need to continue to do the work, even if things are looking like they’re improving. It’s going to take time, and we’re going to have to be social distancing for quite some time, but I hope everyone continues to take precautions and push forward.
Laura Dean (Practical Nursing ’19)
Laura works as a full-time RPN in the Comprehensive Stroke Unit as part of the Trillium Health Partners - Mississauga Hospital.
What does your day to day typically look like?
Almost every patient we have has had some form of stroke, so my day to day can be different depending on which patients I am assigned to. Some patients are fully alert, oriented and independent, and others are completely incapacitated from the stroke. Patients can require total care, or need no assistance at all. Assignments can be heavy when you have multiple patients at different levels of total/assisted care. There are days when a 12-hour day turns into a 15-hour day. These can be very tiring, especially when you get home late and still have a shift the following day. I can say this: I am fortunate enough to work with a great team of people. Everyone helps each other whenever possible. It is a very positive environment and makes the day to day better.
How has your work changed since COVID-19?
Since COVID-19 we now wear masks through our 12-hour shifts, I personally find that this more exhausting than what I normally feel after a regular shift. We have to self screen every morning before arriving at work, and there are designated entrances and exits for staff. Mostly what has changed is the time we now have to spend on the phones giving updates to families who are unable to come in and visit their families. This happens a lot in the stroke unit, as many of our patients have lost the ability to speak, or what they say isn’t quite as clear.
We have also found ourselves with many more patients on precautions as they arrive on our unit and we wait for their COVID-19 test results to come back. One upside to being on the stroke unit has been that if one of our patient’s test results came back positive, then that patient was immediately removed to a COVID-19-designated unit. If you happened to have had contact with that person, you’re normally wearing full PPE, but still had to self monitor for 14 days after contact.
Can you share a story about something or someone that has inspired you during this experience?
There has not been one single incident that has inspired me during this experience, but every one of my patients inspires me every day. I try to treat my patients how I would expect my own family to be treated, should it be them in the patient’s position. I try every day to keep a positive demeanor and outlook for my patients and spend as much time as physically possible with them to ensure that my patients have everything they could possibly need. Regardless of the time I spend with them, they of course still miss their families. My goal every day when I go to work is to hopefully be able to make at least one, if not all of my patients, smile at least once in the day.
What would you like people to know about your experience during this time?
The hardest part of this experience has to be families not being able to visit. Many stroke patients are elderly, and have some form of Alzheimer’s or dementia. Families are very helpful with patients in helping to reorient them and helping with tasks such as encouraging patients with meals. Many of our patients have language barriers, and families are able to interpret for us as to what they need or want. Families tend to be a big part of our patients care and without them it can be very difficult to figure out what they truly need or want.
What’s your favourite aspect of your job?
My favorite aspect of this job is working with my patients, seeing them smile or laugh and at the end of their stay with us, seeing them go home.
Ashley Giorno (Practical Nursing ’19)

Ashley currently works within Halton Healthcare at Oakville Trafalgar Memorial Hospital on the surgical floor.
What does your day-to-day typically look like?
On a day-to-day basis the floor can be very busy due to its high turnover rate with patients. Depending on the patient and the type of surgery, patients can stay anywhere from a few hours to several days.
Typically, I arrive on the floor about 20 minutes before my shift begins, and will go through the Kardex or “Coles Notes” of what is going on with the patients I have been assigned for the day. From there, I receive a report from the previous nurse and start my day by introducing myself to each patient and ensuring I have a full understanding of their needs.
As the day progresses and patients are sent home, new post-operative patients will arrive to the floor and as their nurse, I will complete a head-to-toe assessment, ice checks (i.e. to ensure the anesthetic is leaving the body and feeling is coming back), and vital signs every hour for the first four hours to confirm they’re recovering from surgery.
Another facet of being on a surgical floor is pain control and making sure patients can preform activities of daily living (ADLs) with minimal pain, which will decrease over time. Throughout the day, it is also necessary to reposition patients who are on bedrest, change surgical dressings, and bring any abnormalities to the attention of the physicians assigned to each patient. As a nurse, I also like to talk to my patients and see how they are doing on an emotional level because surgery can be quite daunting. This form of practice also demonstrates to the patient that I am not just there to do my job and leave, but that I care and want to help in any way I can.
How has your work changed since COVID-19?
My work changed dramatically because of COVID-19 since, initially, surgeries were ramped down completely.
With the scaling down of surgeries, the hospital had put in place a redeployment strategy, which reassigned nurses, such as myself, to other units to help out when needed. This enabled the opportunity for growth as a nurse and the knowledge of how units operate, should the pandemic get worse. I have been deployed to medicine floors, cardiology, oncology, and have screened individuals coming into the building. That alone is a big adjustment for any nurse, but for someone who is just beginning their career it can become extremely overwhelming. I have broken down at work several times because of this but have managed to land on my feet and keep going with the help from my 7C family. They are an amazing support system and I am so lucky to have them through such an uncertain and bizarre time.
OTMH also positioned screening stations at every entrance back in March to ensure the safety of those in the building. As a nurse, I am required to wear personal protective equipment (PPE) such as masks and face shields throughout my 12-hour shifts. Also, every pre-operative patient is tested for COVID-19 prior to being sent down for surgery.”
The atmosphere at work (especially in the beginning of the pandemic) was very uncertain and stressful because no one knew what to expect, but it was nice to be able to talk it out with colleagues who understood the emotional rollercoaster I was going through.
Can you share a story about something or someone that’s inspired you during this experience?
One of the more difficult aspects of working during this time is noticing how alone patients can feel.
This tends to add more stress on everyone, because family members are looking to me for updates on loved ones. At times, it doesn’t feel like there’s enough time in the day, because I need to care for all of my patients equally. I’m grateful OTMH has provided iPads to help give patients and families a chance to stay in contact and see one another via video chat. This has boosted morale and allowed patients and families to have reassurance.
What would you like people to know about your experience during this time?
My experience during this time has definitely been overwhelming, tiring, and stressful, because I never know what to expect going into work. However, despite all of that, I am grateful to be a nurse and to be able to help in any way I can. I’m the kind of person who always extends a hand to someone who needs it or will make a fool out of myself to get someone laughing. The world needs more of that, especially in a time like this.
What I’ve learned is how much we all need to depend on one another in order to survive this pandemic. Actions cause a ripple effect, and when one person wears a mask or does something kind, that affects the next person. Being compassionate and acknowledging how others feel can ease the stress of what is going on in the world. As a nurse, I can do this by helping my patients or talking to family members over the phone who can’t visit their loved ones in hospital.
Helpful gestures, such as offering to deliver someone’s groceries, or just reaching out to check on a neighbour, makes a difference. It takes one person to create change and whether that person works in healthcare or not, they can still do their part to
What is your favourite aspect of your job?
I love helping people. It’s something I’ve been doing for as long as I can remember. I love seeing a patient light up with pride when I tell them how well they’re walking, when they just had knee surgery the previous day. I cherish those moments, and I use them to fuel myself to become a better person both personally and professionally.
I also have to mention my 7C family, because they are another reason why I love my job so much. Everyone has embraced and supported me since I started on the floor as a student in May 2019, and they’ve continued to support me after I was hired. I am a better nurse because of each and every one of them. I always feel supported regardless of the situation and am eternally grateful for the guidance each of them has provided because it has allowed me to grow as a nurse and forge my own path. They are an incredible team and are always there to lend a hand or help out when needed. I have worked many jobs in my life, but this one is my all-time favourite.
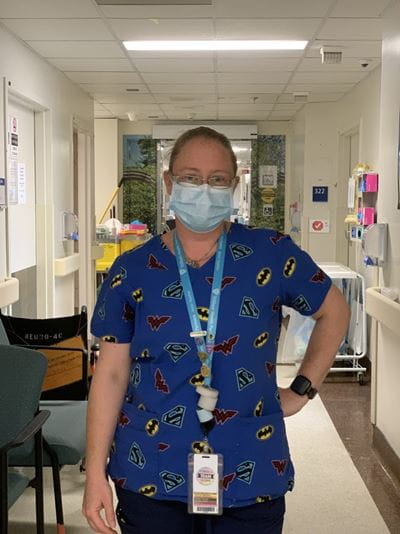
Kellye Janikowski (Practical Nursing ’15)

Kellye currently works as an RPN in the Obstetrical Unit at Milton District Hospital.
What drew you to Sheridan’s Practical Nursing program?
Both my parents were nurses, so I knew what it entailed, but originally, I wanted to get into policing. So I actually took the Police Foundations program at Sheridan before Practical Nursing, and ended up doing fraud investigation for a couple of years. (…) But I was looking for a career change and honestly, was looking for a job with security, and nursing came to mind. I started with General Arts and Sciences for eight months, and if you maintained a certain GPA, you’d get automatic entry into the Practical Nursing Program.
I was actually one of the people that went to the Dominican Republic for my practicum, which was an amazing experience. Their facilities were so far behind compared to North America, but one day – I’ll never forget it for as long as I live – the neurologist at the medical centre told me, “the way we nurse, is that we nurse with love.” That stuck with me for my entire career. You need to have the heart of a nurse to be a successful nurse, and that can’t be taught in any program.
What have your days been like recently?
It’s a little different now, but my typical day starts bright and early at 5 a.m., making a coffee, pulling on my scrubs and throwing my hair in a bun. I’m not doing it anymore, but earlier, I picked up a second job during the pandemic because everyone was looking for nursing. Free coffee at McDonald’s has been getting me through this pandemic. (…) It’s easy to get dehydrated because some days you’re being run off your feet, and it’s harder now because we’re wearing masks all day long so we’re drinking even less. But we do what we can for our patients, and that’s all there is to it. There’s no better feeling in the world than seeing someone who you’ve cared for over 100 days walk out of the hospital. There’s nothing more rewarding than that. I don’t need thank yous from the community – I don’t need posters. That’s enough for me.
What has inspired you during the pandemic?
The nursing community is like family to me, but and we’ve been getting each other through everything right now. We always have each other’s backs. The biggest support system I’ve ever had in my life is my nurse family. When you’re having a bad day, they’ll take over and step up and do what they need to do for your patients. You’re never alone in your assignments.
My friends have also been pretty understanding of what I’m going through and dropping off meals.
What do you do for self care during this time?
At the beginning, I watched a lot of news. Now I avoid it completely. If there’s anything super important, it will be communicated to me through the hospital emails. I also try to stay off social media. I really focus on sleep and nutrition. It can be hard to go to sleep right when I get home, but I’ve been forcing myself to sleep enough, I go for walks and spend time outside when I can. My dog has been amazing – he’s the best hugger ever.
It’s about being conscious of what your limits are and being comfortable talking through your feelings with people. It’s okay to be tired, it’s okay to be sad.
Do you have any advice for current Practical Nursing students?
I hope people want to stay in nursing, even with the pandemic. The pace is totally different, and COVID-19 has changed a lot of the ways we do things, but it’s a great a profession and I love it. I want to tell students that you’ll learn the skills as you go, but always have a good heart and make your patients feel good. People won’t remember if you mess up their IV once or twice – they’ll remember if you sit and chat with them more than once during a 12-hour shift. You have to interact with people and let them know they’re safe and you’re going to help them – don’t make it so clinical and sterile. I know the it can be a bit awkward and scary to talk with people who are sick, but that’s when they need you more than ever. And with COVID-19, they don’t always have families to support them, so we’re their family.
Written by: Meagan Kashty, Digital Communications Officer at Sheridan.
Media Contact
For media inquiries, contact Sheridan’s Communications and Public Relations team.





